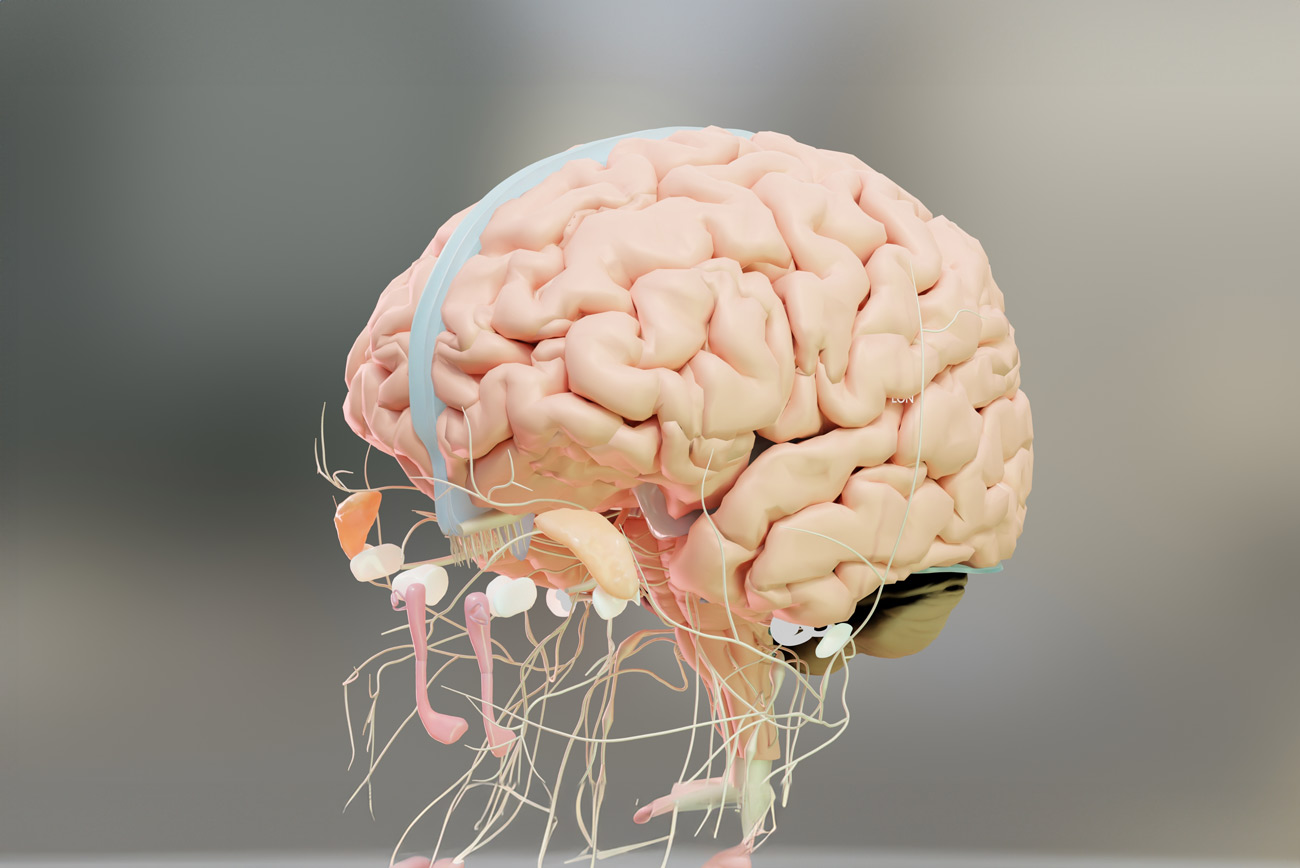
Understanding the Nervous System: The Body’s Response Hub
The nervous system is the command center of our body. It governs everything from heartbeat and breathing to emotions and memory. In moments of calm, it allows us to rest, digest, and connect with others. In moments of stress, it shifts gears to protect us.
Our nervous system constantly scans the world for cues of safety or danger, often below conscious awareness. This automatic process — known as neuroception — determines whether we feel relaxed, alert, anxious, or shut down. Understanding this system helps explain why our reactions differ so much from person to person.
The Three Main States of the Nervous System
According to polyvagal theory, developed by Dr. Stephen Porges, our nervous system operates on three main levels:
- Fight or Flight (Sympathetic Activation) When the brain perceives a threat, the body mobilizes. Heart rate increases, muscles tense, and adrenaline surges. You may feel restless, irritable, or anxious — ready to take action or escape danger.
- Freeze or Shutdown (Dorsal Vagal Response) When stress feels overwhelming or inescapable, the body may shut down to conserve energy. This can look like numbness, disconnection, fatigue, or feeling “spaced out.” It’s the nervous system’s way of saying, “I can’t handle this right now.”
- Rest, Digest, and Connect (Ventral Vagal Activation) This is the state of safety, calm, and connection. Here, we can think clearly, engage socially, and experience joy or creativity. Healing happens most effectively in this state.
Our nervous systems move between these states throughout the day — they’re not static. The goal isn’t to stay calm all the time, but to develop flexibility — the ability to return to balance after stress.
The Science of Safety: Why It Feels Different for Everyone
No two nervous systems are alike. Even if two people share similar experiences, their internal responses can be worlds apart. What feels safe to one might feel stressful to another.
Several factors influence this:
- Early experiences and attachment patterns — How we were soothed or supported as children shapes how we handle stress as adults.
- Trauma and chronic stress — Repeated exposure to overwhelm can sensitize the nervous system, making it quicker to activate.
- Cultural and family dynamics — How emotions and vulnerability are expressed (or not expressed) in your culture deeply affects your comfort with support.
- Health and biology — Genetics, hormones, and even gut health can alter how our body processes stress.
For example, imagine two coworkers experiencing workplace tension. One might respond by talking things out immediately (ventral vagal — connection), while the other shuts down and avoids confrontation (dorsal vagal — protection). Both responses make sense for their individual systems.
The takeaway? There’s no “right” way to respond to stress. Your nervous system is always doing its best to protect you, even when it feels confusing or inconvenient.
Why Support Feels Different for Each Nervous System
Because each nervous system interprets the world through its own lens, the kind of support that truly helps must be equally individualized.
Example 1: The Quiet Seeker vs. The Connector
After a stressful day, one person might crave solitude — curling up in bed to rest. Their body finds safety in stillness. Another person might call a close friend, needing laughter and company to release tension. Their body finds safety in connection.
Both are right. Both are healing.
Example 2: Trauma Triggers and Safety Cues
For someone with a history of emotional neglect, offers of support might feel suspicious or uncomfortable. Their nervous system has learned that closeness can sometimes hurt. In contrast, someone who grew up with consistent care might immediately relax when offered help.
Recognizing these nuances allows us to respond without judgment — to offer empathy instead of “fixing.” It also invites us to ask ourselves: What does safety feel like in my body? What helps me soften and breathe easier?
Personalized Support: Meeting the Nervous System Where It Is
Effective support begins with meeting the nervous system where it is, not where we think it “should” be. This is at the heart of trauma-informed care — the practice of responding with awareness, choice, and compassion.
Step 1: Notice the State
Is the person energized and tense (fight/flight)? Withdrawn or numb (freeze)? Or open and connected (rest/digest)? Identifying this helps guide the kind of support that will feel safe.
Step 2: Offer Support That Matches the State
- In fight or flight, grounding or rhythmic movement can help discharge excess energy — walking, shaking out the arms, or breathing in rhythm.
- In freeze, gentle stimulation like warmth, sensory grounding, or small movements can help the body slowly re-engage.
- In rest and digest, connection and conversation often deepen healing.
Step 3: Prioritize Consent and Choice
For someone in survival mode, even well-intentioned help can feel intrusive. Ask simple questions like, “Would you like to talk, or would quiet company feel better right now?” These choices empower the person’s nervous system to relax.
This approach shifts support from “doing” to being with — from fixing to witnessing. Healing unfolds when the body feels seen, not pressured.
How to Recognize Your Own Nervous System Cues
Learning your nervous system’s patterns is a powerful step toward emotional resilience. Start by tuning into the body’s signals before they escalate.
- When your heart races or your breathing becomes shallow, your system may be moving into fight or flight.
- When you feel disconnected, heavy, or foggy, that’s often freeze or shutdown.
- When you feel present, curious, and safe, you’re in ventral vagal — the zone of connection.
Keeping a “body awareness journal” can help you notice these shifts. Ask:
- What triggered this feeling?
- What sensations do I notice?
- What helps me return to balance?
Over time, this awareness builds self-compassion — you begin to understand that your reactions aren’t “bad,” they’re protective.
Co-Regulation: The Power of Shared Calm
Humans are wired for connection. From infancy, our nervous systems learn to regulate through others — through tone of voice, eye contact, and gentle presence. This process is called co-regulation, and it remains essential throughout life.
When we’re around someone who feels grounded and compassionate, our body naturally mirrors that calm. Likewise, when we’re surrounded by anxiety or tension, our nervous system can absorb it. This is why who we spend time with matters for emotional health.
Simple Ways to Co-Regulate
- Share calm, not advice. Instead of “You’re overreacting,” try “I’m here with you.”
- Breathe together. Slow, steady breathing signals safety to both bodies.
- Use gentle tone and soft facial expressions. Safety is communicated through the senses.
- Engage in shared rhythm. Walking, cooking, or listening to music together can synchronize nervous systems.
- Respect boundaries. Co-regulation only works when both people feel safe and willing.
Co-regulation reminds us that healing isn’t a solo journey. Sometimes, the most powerful medicine is presence — the quiet assurance that we don’t have to face the storm alone.
Self-Regulation: Building Inner Resilience
While connection helps us calm, true empowerment comes from learning how to self-regulate — to guide our own nervous system back to safety.
Tools for Self-Regulation
- Grounding Through the Senses
- Notice five things you can see, four you can touch, three you can hear, two you can smell, one you can taste.
- This anchors you in the present moment.
- Movement and Breath
- Gentle yoga, stretching, or a mindful walk can release tension.
- Try box breathing (inhale 4, hold 4, exhale 4, hold 4).
- Creative Expression
- Art, journaling, singing, or dancing help the body express what words can’t.
- Soothing Routines
- Lighting a candle, sipping tea, or having a nightly wind-down ritual can train your body to anticipate calm.
- Affirmations of Safety
- Whisper to yourself: “I’m safe right now.” “My body knows how to return to balance.”
The Key Is Curiosity, Not Perfection
Self-regulation is not about staying calm all the time — it’s about noticing when you’re activated and responding with kindness. Each small moment of awareness strengthens your nervous system’s capacity to adapt and recover.
Breaking Free from Comparison
Modern wellness culture often sends mixed messages: You should meditate. You should journal. You should just relax. But when those tools don’t work for us, we can feel like we’re failing at self-care.
The truth is, there is no universal formula for regulation. What matters isn’t the method, but whether it helps your body feel safe and alive.
Letting Go of “Shoulds”
- Meditation may be calming for some, but activating for others.
- Journaling may bring clarity, or it may intensify rumination.
- Group settings may offer connection — or overwhelm the senses.
When we stop comparing our coping to others, we open the door to real healing. There’s freedom in saying, “This works for me, and that’s enough.”
The Role of Professional Support
Sometimes, the nervous system needs specialized support to heal from patterns rooted in trauma or chronic stress. This is where therapy becomes a powerful ally.
At Joy Spring Mental Health, our trauma-informed therapists integrate modalities like:
- Somatic therapy — using body awareness to release stored tension and trauma.
- EMDR (Eye Movement Desensitization and Reprocessing) — reprocessing distressing memories in a safe, guided way.
- Polyvagal-informed therapy — helping clients recognize and shift their nervous system states.
- Mindfulness-based therapy — strengthening present-moment awareness and emotional regulation.
Therapy as a Relationship of Safety
In therapy, the goal isn’t to “fix” you — it’s to support your nervous system in feeling safe enough to heal. Together, you and your therapist create a space where the body can finally relax its defenses, explore emotions, and integrate experiences with compassion.
Over time, clients learn to recognize their triggers, develop new coping strategies, and experience a deeper sense of trust — in themselves, in their bodies, and in connection with others.
Everyday Ways to Support Your Nervous System
Healing doesn’t have to happen only in therapy sessions. Daily, mindful practices help reinforce safety and balance. The goal isn’t perfection — it’s awareness and consistency.
Gentle, Everyday Practices
- Create Rhythms of Rest and Activity Alternate between effort and rest — work, then breathe; connect, then pause.
- Move Mindfully Explore yoga, tai chi, dancing, or simply stretching your body in ways that feel good. Movement is medicine.
- Spend Time in Nature Natural environments reset the nervous system. Listen to birds, touch the ground, feel the air.
- Set Boundaries That Protect Energy It’s okay to say no. Boundaries aren’t barriers — they’re invitations to safety.
- Practice Gratitude or Reflection Gratitude shifts the brain’s focus toward safety and abundance, calming the stress response.
- Cultivate Safe Relationships Healing happens in connection. Seek spaces where you feel seen, not judged.
- Limit Overstimulation Reduce sensory overload — dim lights, take tech breaks, slow down transitions between tasks.
- Prioritize Sleep and Nourishment A rested, well-fed body can better regulate emotions. Self-care is physiological, not just emotional.
The Myths About Regulation
To deepen understanding, it helps to debunk a few common myths:
- Myth 1: Regulation means feeling calm all the time. Truth: Regulation means flexibility — moving through stress and returning to balance.
- Myth 2: If I were stronger, I wouldn’t get triggered. Truth: Triggers are nervous system responses, not character flaws.
- Myth 3: I can think my way out of stress. Truth: The body must feel safe for the mind to follow. Regulation starts in the body.
- Myth 4: Healing means never feeling anxious again. Truth: Healing means relating to anxiety differently — with compassion, not fear.
The Power of Awareness and Compassion
As we deepen our understanding of the nervous system, we begin to see stress responses not as failures but as protective strategies. Each reaction — fight, flight, freeze, fawn — once kept us safe. Awareness allows us to thank those parts of ourselves and invite new patterns of safety.
Healing happens through compassionate curiosity — the willingness to explore without judgment. The nervous system learns safety through repetition and kindness, not through force or shame.
Honoring the Nervous System’s Wisdom
Support looks different for every nervous system because every human carries a unique story. What feels comforting to one may overwhelm another — and that’s okay. When we understand that our responses are shaped by biology, experience, and environment, we move from self-blame to self-compassion.
At Joy Spring Mental Health, we believe that healing begins by listening to the body’s wisdom. Each breath, heartbeat, and pause offers information about what we need. Whether through therapy, community, or daily self-care, the goal is not to be perfect — but to be present.
When we stop comparing and start listening — to our bodies, to each other, and to our nervous systems — support becomes not just possible, but deeply transformative.